There's a link between ADHD and PTSD, suggesting that individuals with ADHD are at elevated risk for PTSD and vice versa.
Research states that people with ADHD are four times more likely to have PTSD than those without ADHD. Furthermore, individuals with PTSD are twice as likely to have ADHD.
ADHD and PTSD can present similarly, with impaired impulse control (the ability to stop yourself from engaging in certain behaviors), irritability, and anxiety.
The most significant difference between ADHD and PTSD is that PTSD symptoms are the result of a traumatic experience and can get triggered by flashbacks thereof. By contrast, ADHD is a neurological and developmental disorder that's most often diagnosed in childhood.
By treating ADHD, you might be able to also better focus on your PTSD treatments, and working on PTSD might lessen the anxiety and restlessness caused by ADHD.
Experiencing trauma can be a life-altering experience. Trauma can shape how we grow and develop, how we perceive ourselves, and how we make sense of the world.
In fact, a traumatic event or a series of events can, in some cases, progress to post-traumatic stress disorder (PTSD), an anxiety disorder characterized by feelings of guilt, isolation, irritability, difficulty sleeping, or difficulty concentrating.
These symptoms can interfere with our daily lives and leave us feeling absent-minded, forgetful, easily distracted, and confused.
But most of these symptoms also fall under the category of a different disorder: attention deficit hyperactivity disorder (ADHD), a neuro-behavioral disorder characterized by an ongoing pattern of inattention and/or hyperactivity/impulsivity.
Complicating matters further, ADHD and PTSD sometimes also occur together. So how do you recognize which disorder is at the core of your symptoms and what happens when a person with ADHD experiences a traumatic event?
In addition to answering those questions, we’ll also answer the following:
1) Can you have ADHD and PTSD at the same time?
2) What is the link between ADHD and trauma?
3) What are the symptoms of PTSD and ADHD overlap?
4) How can you tell the difference between ADHD and PTSD?
5) Can PTSD make ADHD symptoms worse?
6) What’s the treatment for ADHD and PTSD combined?
Can You Have ADHD and PTSD at the Same Time?
According to research, there's a link between ADHD and PTSD, suggesting that individuals with ADHD are at elevated risk for PTSD and vice versa.
In fact, people with ADHD are four times more likely to have PTSD than those without ADHD. Furthermore, individuals with PTSD are twice as likely to have ADHD.
But why is that?
What’s the Link Between ADHD and PTSD?
If someone has ADHD, they might be at risk for exposure to traumatic experiences, in particular during adolescence. This is because ADHD is associated with high levels of risk-taking behaviors and impulsivity that could lead to traumatic events.
On the other hand, early-life trauma could trigger ADHD symptoms. The link is probably caused by toxic stress, which is the outcome of persistent activation of the body's stress response system that’s typical for trauma.
Still, timing plays a key role here. Since ADHD is a neurodevelopmental condition – meaning that it starts early during development – trauma that doesn’t occur in childhood is unlikely to trigger ADHD later in life. Of note, there are many factors associated with ADHD, both genetic and environmental, that need to be considered in order to understand its cause.
What Are the Symptoms of PTSD and ADHD Overlap?
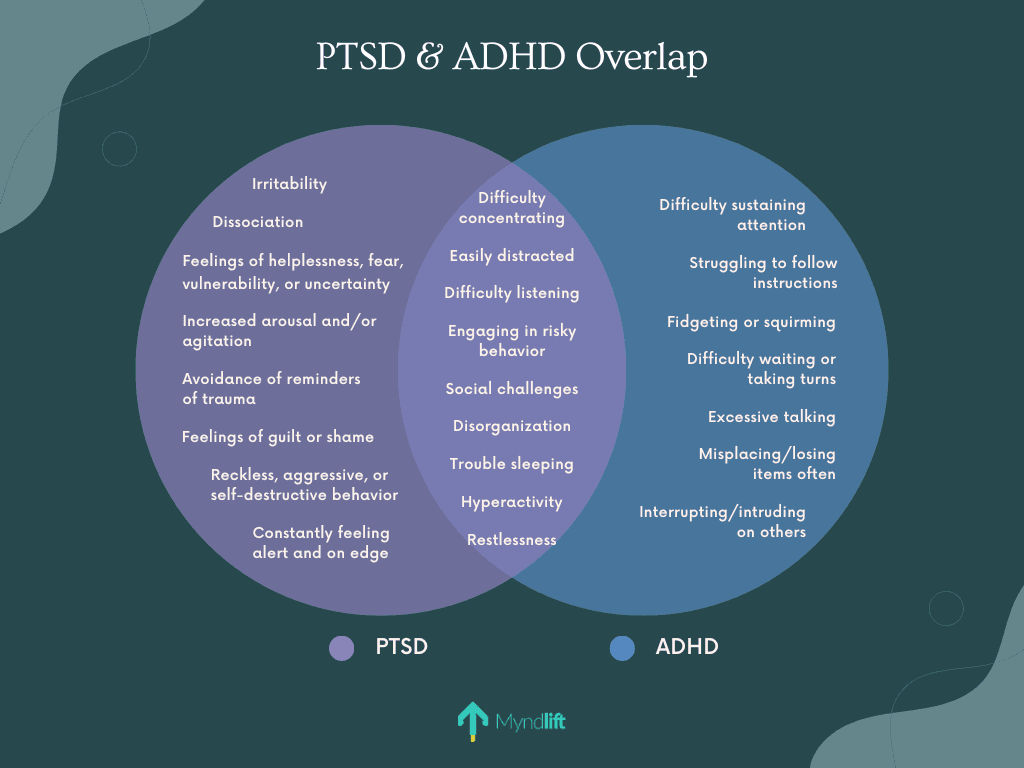
ADHD and PTSD can present similarly, with impaired impulse control (the ability to stop yourself from engaging in certain behaviors), irritability, and anxiety. In fact, some of the most common overlapping symptoms are:
Struggling to stay focused on tasks: If you have ADHD, you probably have lower levels of dopamine and norepinephrine, which are neurotransmitters associated with attention and focus. And if you also have PTSD, you may have trouble paying attention because your body is producing excessive amounts of cortisol, the stress hormone, which makes it hard to focus.
Engaging in risky behaviors: In an ADHD brain, the prefrontal cortex (the part of the brain that helps us to control and override impulsive urges) and the thalamus, a brain area that sends signals to many brain regions, including the frontal cortex, function abnormally. This can then result in impulsive behavior and difficulty regulating states of arousal. On the other hand, PTSD can make you more likely to engage in risky behaviors in an attempt to distract yourself from high emotional states.
Social challenges: Sometimes, having ADHD makes it hard to pick up on social cues or take turns in conversations. In addition, some ADHD symptoms can be misinterpreted, making it challenging to find and maintain connections with others. For example, your friends might interpret inattention as shyness or impulsiveness as aggression. Similarly, hyperarousal (being more sensitive and overly responsive to stimuli and events) which is a common PTSD symptom, can also impact close relationships.
How Can You Tell the Difference Between ADHD and PTSD Symptoms?
Even though there's an overlap between ADHD and PTSD, the most significant difference between the two conditions is that PTSD symptoms are the result of a traumatic experience and can get triggered by flashbacks thereof.
By contrast, ADHD is a neurological and developmental disorder that's most often diagnosed in childhood. It's typically present from birth, though its symptoms become more prevalent when life demands exceed capacity (for example, when a child starts school or when the workload becomes more intense as an adult).
When looking at the symptoms, mental health professionals usually ask questions about when the first signs started, how much impact they have on your life, and if they've been present lifelong or if they began after a specific (traumatic) event.
Note that trying to differentiate ADHD or trauma-related symptoms on your own can lead to delays in care, which can lead to worsening symptoms, so it's best to consult with a mental health professional in order to gain full clarity.
Can PTSD Make ADHD Symptoms Worse?
If you have both conditions, the symptoms tend to exacerbate one another. For example, studies have shown that experiencing a traumatic event may be a risk factor for both the development and persistence of ADHD symptoms into adulthood.
Depending on the nature of the trauma, children and adults with ADHD can also have trouble in social relationships or more struggles at work, which can all exacerbate ADHD-related symptoms.
That is why we strongly encourage reaching out to a mental health professional for help in order to prevent symptoms from getting worse. This brings us to our next question.
What’s the Treatment for ADHD and PTSD Combined?
The first step in alleviating both PTSD and ADHD symptoms is receiving a proper diagnosis. Moreover, when being assessed for ADHD, you should also be screened for a history of PTSD, and vice versa. If the disorders co-occur, evaluating and treating both is considered the most effective approach.
For example, by treating ADHD, you might be able to also better focus on your PTSD treatments, and working on PTSD might lessen the anxiety and restlessness caused by ADHD.
Treatment for ADHD and PTSD typically includes medication, therapy, or a combination of both. But there are also lifestyle changes and different types of therapy that can help you manage both conditions, such as neurofeedback and/or meditation.
Regardless of your type of therapy, try to stay consistent and aware that the therapeutic process isn't an overnight fix. It's a process of learning, growing, and making small changes that hopefully become long-lasting. With the proper mental health tools and support, you’ll not only be able to live with both ADHD and PTSD, you’ll be able to thrive!
Myndlift provides a personalizedexpert-guided brain training program that can help you achieve your goals towards reaching improved focus and calm. Check if you’re eligible to kick start your journey with us for better brain health from here.
About the author:
Dubravka Rebic
Dubravka Rebic puts a lot of time and energy into researching and writing in order to help create awareness and positive change in the mental health space. From poring over scientific studies to reading entire books in order to write a single content piece, she puts in the hard work to ensure her content is of the highest quality and provides maximum value.
About the checker:
Carola Tuerk, Ph.D.
Carola is a cognitive neuroscientist and a scientific consultant for Myndlift. In her research, she is particularly interested in how early life experiences shape brain development and mental health with a particular focus on children. She has obtained a BSc in psychology, an MSc in neuroscience, and a PhD in cognitive neuroscience and is passionate about brain health. In her free time, Carola likes to exercise or play music to relax.
References
Spencer AE, Faraone SV, Bogucki OE, Pope AL, Uchida M, Milad MR, Spencer TJ, Woodworth KY, Biederman J. Examining the association between posttraumatic stress disorder and attention-deficit/hyperactivity disorder: a systematic review and meta-analysis. J Clin Psychiatry. 2016 Jan;77(1):72-83. doi: 10.4088/JCP.14r09479. PMID: 26114394.
Ford, J.D., Connor, D.F. ADHD and posttraumatic stress disorder. Curr Atten Disord Rep 1, 60–66 (2009). https://doi.org/10.1007/s12618-009-0009-0
Vrijsen JN, Tendolkar I, Onnink M, Hoogman M, Schene AH, Fernández G, van Oostrom I, Franke B. ADHD symptoms in healthy adults are associated with stressful life events and negative memory bias. Atten Defic Hyperact Disord. 2018 Jun;10(2):151-160. doi: 10.1007/s12402-017-0241-x. Epub 2017 Oct 28. PMID: 29081022; PMCID: PMC5973996.
Millichap JG. Etiologic classification of attention-deficit/hyperactivity disorder. Pediatrics. 2008 Feb;121(2):e358-65. doi: 10.1542/peds.2007-1332. PMID: 18245408.
Del Campo N, Chamberlain SR, Sahakian BJ, Robbins TW. The roles of dopamine and noradrenaline in the pathophysiology and treatment of attention-deficit/hyperactivity disorder. Biol Psychiatry. 2011 Jun 15;69(12):e145-57. doi: 10.1016/j.biopsych.2011.02.036. Epub 2011 May 6. PMID: 21550021.
Elzinga, B., Schmahl, C., Vermetten, E. et al. Higher Cortisol Levels Following Exposure to Traumatic Reminders in Abuse-Related PTSD. Neuropsychopharmacol 28, 1656–1665 (2003). https://doi.org/10.1038/sj.npp.1300226
Teresa Bailey & Arthur Joyce (2015) The Role of the Thalamus in ADHD Symptomatology and Treatment, Applied Neuropsychology: Child, 4:2, 89-96, DOI: 10.1080/21622965.2015.1005475
Arnsten AF. The Emerging Neurobiology of Attention Deficit Hyperactivity Disorder: The Key Role of the Prefrontal Association Cortex. J Pediatr. 2009 May 1;154(5):I-S43. doi: 10.1016/j.jpeds.2009.01.018. PMID: 20596295; PMCID: PMC2894421.
Weiss NH, Tull MT, Viana AG, Anestis MD, Gratz KL. Impulsive behaviors as an emotion regulation strategy: examining associations between PTSD, emotion dysregulation, and impulsive behaviors among substance dependent inpatients. J Anxiety Disord. 2012 Apr;26(3):453-8. doi: 10.1016/j.janxdis.2012.01.007. Epub 2012 Feb 6. PMID: 22366447; PMCID: PMC3305816.
Beck JG, Grant DM, Clapp JD, Palyo SA. Understanding the interpersonal impact of trauma: contributions of PTSD and depression. J Anxiety Disord. 2009 May;23(4):443-50. doi: 10.1016/j.janxdis.2008.09.001. Epub 2008 Sep 18. PMID: 18986792; PMCID: PMC2682342.
Vrijsen JN, Tendolkar I, Onnink M, Hoogman M, Schene AH, Fernández G, van Oostrom I, Franke B. ADHD symptoms in healthy adults are associated with stressful life events and negative memory bias. Atten Defic Hyperact Disord. 2018 Jun;10(2):151-160. doi: 10.1007/s12402-017-0241-x. Epub 2017 Oct 28. PMID: 29081022; PMCID: PMC5973996.